TRAUMATIC BRAIN INJURY
Traumatic brain injury (TBI) – considered the most complex disease in the most complex organ – remains a major public health problem worldwide and is the leading cause of death and disability among young adults in developed countries. Each year an estimated 250,000 Americans are hospitalized after suffering a severe TBI, and 50,000 Americans will die as a result of these injuries. Despite these numbers, there is still no treatment for TBI or drug that is able to improve neurologic recovery. Since 1980, no less than 35 large-scale clinical trials have been conducted on new therapies or drugs, but all have failed to show benefit for patients. Why?
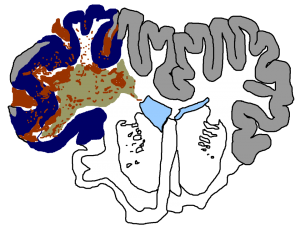
There is good reason to believe the past approach to clinical trials in TBI has been wrong. In these trials, TBI is treated as a single disease entity and all patients are given the same drug and dosing. However, we now appreciate more than ever that TBI is heterogeneous and multi-factorial, consisting of a mix of pathologic processes that can be active in different patients and in different regions of the brain. Thus, a treatment that may work for one patient might not work for another. Future approaches must be based on identifying particular processes active in individual patients and implementation of therapies to target them. This is the personalized, precision medicine required for a disease like TBI.
Unfortunately, past approaches to treatment discovery in TBI have relied too heavily on pre-clinical models of TBI disease processes. Under this paradigm, it is assumed that discoveries made in the laboratory will also apply to the human condition, and, as a further leap, will apply equally to all patients. Often these assumptions are not tested in clinical studies, in part because our ability to monitor the brain after TBI, as patients struggle to regain consciousness and decline neurologically, remains limited. To date, intermittent CT (computed tomography) imaging remains the cornerstone of TBI diagnostics, but often imaging only reveals damage that has already occurred, when the opportunity for intervention has passed.
Thus, the new clinical science of spreading depolarizations lays the foundation for a paradigm shift in TBI that overcomes the pitfalls of past approaches and delivers personalized, targeted treatment for this challenging disease. With signals up to 20-times larger than brain seizures, spreading depolarizations are a process that can be measured in real-time in individual patients. And studies have shown that spreading depolarizations occur in many, but not all patients, confirming the clinical relevance and revealing a major source of disease heterogeneity.
If safe and effective treatments to block these harmful waves are found, patients can then be treated on an individualized basis. In clinical trials, individual patient monitoring would allow for a ‘selective inclusion’ approach in which only patients exhibiting the targeted pathologic process – spreading depolarizations – would be treated. Furthermore, therapeutic dosing and duration could be tailored to their effect on the monitored brain processes. In past TBI research, there has never been a clinical trial in which a pathologic neuronal process was measured as a condition for selective, targeted neuroprotective drug treatment.