ANEURYSM / SUBARACHNOID HEMORRHAGE
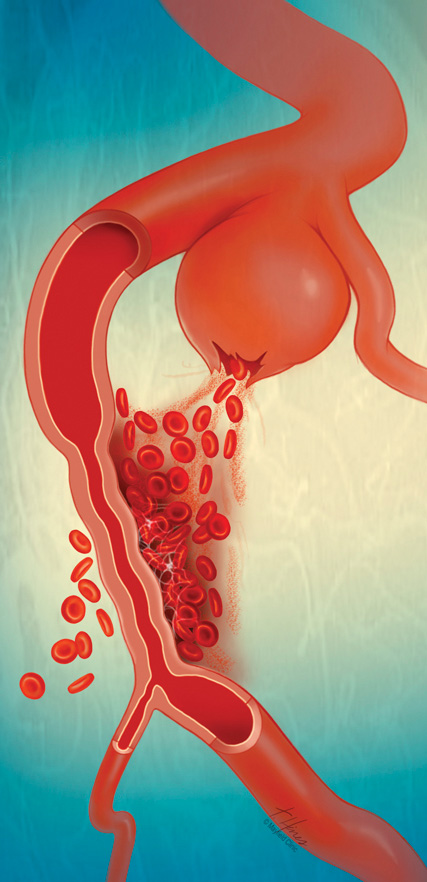
Aneurysmal subarachnoid hemorrhage (aSAH) is the second most common type of hemorrhagic stroke, and results from rupture of a basal cerebral artery aneurysm. The blood leaves the cerebral circulation and accumulates in the subarachnoid space covering the brain surface. Delayed cerebral ischemia (DCI) is the most prominent in-hospital complication after aSAH and is presumably caused by breakdown of erythrocyte products in the subarachnoid space. The clinical signs of DCI are global and focal neurological deficits which lead to significant deterioration in functional outcome (Vergouwen et al 2010). In electrocorticographic (ECoG) recordings, clusters of recurrent spreading depolarizations (SDs) with prolonged depression of the spontaneous activity indicate the occurrence of DCI (Dreier et al 2006).
DCI represents a model disease for hypoxic-ischemic injury for two reasons (Dreier 2011). First, it occurs with a peak incidence around day seven after the initial hemorrhage while the patient is already on the neurocritical care unit. In animal experiments, neuroprotectants have been found to be most effective either when given within minutes after the onset of acute neuronal injury or when they have been preadministered. Thus, DCI allows us to treat patients with a neuroprotectant before the possible insult or very shortly thereafter to prove or disprove the neuroprotective concept. Second, neurosurgical procedures are indicated in patients early after the initial hemorrhage, allowing implantation of invasive probes. This provides the unique option to invasively monitor the whole period of ischemic stroke development in patients, to perform early treatment stratification according to the presence or absence of biomarkers such as SDs sensed in real time by neuromonitoring devices, and then record the parenchymal response to the neuroprotectant.
In 2017, COSBID showed in a translational study that clotted blood on the brain surface is sufficient to trigger SD clusters and early infarcts in a swine model, and that phenomenologically, nearly identical early neuromonitoring and neuroimaging findings occur in patients (Hartings et al 2017). In 2018, using neuromonitoring technology in combination with longitudinal neuroimaging, the entire sequence of both early and delayed brain infarct development after aSAH with SD-induced persistent activity depression, SD-induced spreading ischemias, and the transition of clustered SDs to the negative ultraslow potential (NUP) was demonstrated in a small patient population in which optoelectrodes were directly overlying newly developing infarcts (Dreier et al 2018). In the same year, the first-of-its-kind 50-patient treatment study of spreading ischemia after aSAH with cilostazol was published (Sugimoto et al 2018). This study showed a trend for less DCI in the cilostazol group. Correspondingly, the total SD-induced depression duration per recording day and the occurrence of isoelectric SDs were significantly lower in the cilostazol group. In 2022, DISCHARGE-1, the first COSBID sub-study of larger scale on SDs and aSAH, was published (Dreier et al 2022). DISCHARGE-1 found that the average patient admitted to the neurocritical care unit after aneurysm treatment had already lost 46±73ml of brain tissue due to early focal brain damage and lost an additional 36±80ml (44% of the total focal brain damage) over the next two weeks because of delayed ischemic infarcts. In this prospective, observational, multicenter, cohort, diagnostic phase III trial in 180 aSAH patients, SD variables were included in each multiple regression model for longitudinal neuroimaging-proven early, delayed, and total brain damage, outcome at 7 months, and patient death, strongly suggesting that SDs are an independent biomarker of progressive brain injury.
Dreier JP. 2011. The role of spreading depression, spreading depolarization and spreading ischemia in neurological disease. Nat Med 17:439-447. DOI: 10.1038/nm.2333
Dreier JP, Winkler MKL, Major S, Horst V, Lublinsky S, Kola V, Lemale CL, Kang EJ, Maslarova A, Salur I, Luckl J, Platz J, Jorks D, Oliveira-Ferreira AI, Schoknecht K, Reiffurth C, Milakara D, Wiesenthal D, Hecht N, Dengler NF, Liotta A, Wolf S, Kowoll CM, Schulte AP, Santos E, Guresir E, Unterberg AW, Sarrafzadeh A, Sakowitz OW, Vatter H, Reiner M, Brinker G, Dohmen C, Shelef I, Bohner G, Scheel M,
Vajkoczy P, Hartings JA, Friedman A, Martus P, Woitzik J. 2022. Spreading depolarizations in ischaemia after subarachnoid haemorrhage, a diagnostic phase III study. Brain 145:1264-1284. DOI: 10.1093/brain/awab457.
Dreier JP, Woitzik J, Fabricius M, Bhatia R, Major S, Drenckhahn C, Lehmann TN, Sarrafzadeh A, Willumsen L, Hartings JA, Sakowitz OW, Seemann JH, Thieme A, Lauritzen M, Strong AJ. 2006. Delayed ischaemic neurological deficits after subarachnoid haemorrhage are associated with clusters of spreading depolarizations. Brain 129:3224-3237. DOI: 10.1093/brain/awl297.
Hartings JA, York J, Carroll CP, Hinzman JM, Mahoney E, Krueger B, Winkler MKL, Major S, Horst V, Jahnke P, Woitzik J, Kola V, Du Y, Hagen M, Jiang J, Dreier JP. 2017. Subarachnoid blood acutely induces spreading depolarizations and early cortical infarction. Brain 140:2673-2690. DOI: 10.1093/brain/awx214.
Luckl J, Lemale CL, Kola V, Horst V, Khojasteh U, Oliveira-Ferreira AI, Major S, Winkler MKL, Kang EJ, Schoknecht K, Martus P, Hartings JA, Woitzik J, Dreier JP. 2018. The negative ultraslow potential, electrophysiological correlate of infarction in the human cortex. Brain 141:1734-1752. DOI: 10.1093/brain/awy102.
Sugimoto K, Nomura S, Shirao S, Inoue T, Ishihara H, Kawano R, Kawano A, Oka F, Suehiro E, Sadahiro H, Shinoyama M, Oku T, Maruta Y, Hirayama Y, Hiyoshi K, Kiyohira M, Yoneda H, Okazaki K, Dreier JP, Suzuki M. 2018. Cilostazol decreases duration of spreading depolarization and spreading ischemia after aneurysmal subarachnoid hemorrhage. Ann Neurol 84:873-885. DOI: 10.1002/ana.25361.
Vergouwen MD, Vermeulen M, van Gijn J, Rinkel GJ, Wijdicks EF, Muizelaar JP, Mendelow AD, Juvela S, Yonas H, Terbrugge KG, Macdonald RL, Diringer MN, Broderick JP, Dreier JP, Roos YB. 2010. Definition of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage as an outcome event in clinical trials and observational studies: proposal of a multidisciplinary research group. Stroke 41:2391-2395. DOI: 10.1161/STROKEAHA.110.589275.
